New Horizons in Cancer Immunotherapy Trials
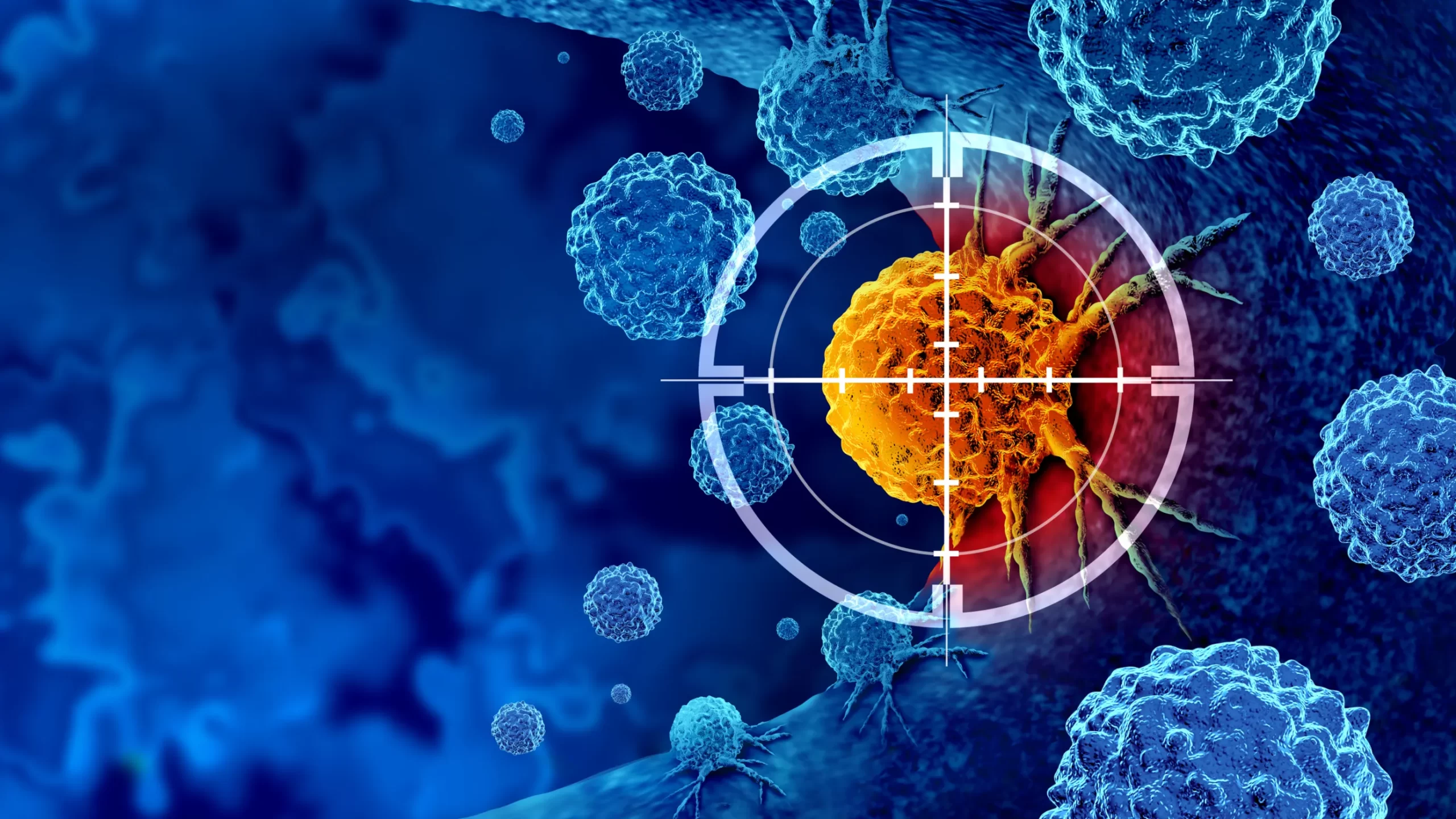
Cancer immunotherapy has redefined the landscape of oncology, offering new hope where conventional therapies often fall short. By harnessing the power of the body’s own immune system, immunotherapy has demonstrated durable responses across a variety of cancers. However, despite these advances, challenges remain—particularly regarding response variability, toxicity, and resistance.
Today, innovative strategies and trial designs are paving the way for the next generation of immunotherapies. Let’s explore the new horizons in cancer immunotherapy trials and the transformative potential they hold.
The Evolution of Cancer Immunotherapy
The past decade has seen remarkable successes with immune checkpoint inhibitors, chimeric antigen receptor (CAR) T-cell therapies, and cancer vaccines. Agents targeting CTLA-4, PD-1, and PD-L1 have become standard treatments for cancers like melanoma, lung cancer, and renal cell carcinoma.
Yet, only a subset of patients experiences long-term benefits, and resistance—either primary or acquired—remains a formidable hurdle. This has driven a surge in innovative clinical trials aiming to broaden the scope and efficacy of immunotherapy.
Emerging Strategies in Immunotherapy Trials
1. Personalized Cancer Vaccines
Cancer vaccines are moving from “one-size-fits-all” approaches to personalized vaccines that target neoantigens—mutations unique to an individual’s tumor. Early-phase trials in melanoma and glioblastoma have shown promising immune responses, igniting interest in expanding this approach across multiple tumor types.
2. Bispecific Antibodies
Bispecific T-cell engagers (BiTEs) are engineered antibodies that simultaneously bind cancer cells and T-cells, directing the immune attack more precisely. New trials are testing bispecifics against hematologic malignancies and solid tumors, offering a potent weapon against cancers that evade traditional therapies.
3. Next-Generation CAR-T and CAR-NK Cells
While CAR-T therapy has revolutionized treatment for certain blood cancers, challenges like cytokine release syndrome and limited success in solid tumors persist. Researchers are developing:
-
Armored CAR-T cells with enhanced resistance to the immunosuppressive tumor microenvironment.
-
CAR-NK cell therapies, which offer lower toxicity and the potential for “off-the-shelf” products, addressing manufacturing and cost barriers.
4. Targeting the Tumor Microenvironment
Innovative trials are focusing on modulating the tumor microenvironment (TME)—the ecosystem of immune cells, blood vessels, and structural components that often suppress immune responses. Strategies include:
-
Inhibitors of immunosuppressive cells (e.g., Tregs, myeloid-derived suppressor cells)
-
Agents targeting stromal barriers to improve immune cell infiltration
5. Combining Immunotherapies
Combination regimens—pairing immune checkpoint inhibitors with chemotherapy, radiation, targeted therapies, or other immunotherapies—are gaining momentum. Rational combinations aim to overcome resistance mechanisms and amplify anti-tumor immunity.
Innovative Clinical Trial Designs
Adaptive Trial Designs
Adaptive trials allow modifications to the study protocol based on interim results, enabling faster identification of effective treatments. This approach is particularly valuable in immunotherapy, where biological responses can be unpredictable.
Biomarker-Driven Trials
Precision medicine is at the heart of modern immunotherapy trials. Biomarkers such as tumor mutational burden (TMB), microsatellite instability (MSI), and PD-L1 expression are guiding patient selection to optimize therapeutic outcomes.
Decentralized and Digital Trials
Remote monitoring through digital tools is enabling broader patient participation in immunotherapy trials. Real-time data collection improves patient engagement and provides a more comprehensive understanding of treatment effects over time.
Challenges and Considerations
Despite these promising developments, several challenges persist:
-
Managing immune-related adverse events (irAEs) remains critical.
-
Standardizing biomarker assays and validation is essential for reproducibility.
-
Achieving durable responses in “cold” tumors—those lacking immune cell infiltration—requires novel therapeutic strategies.
Regulatory agencies are increasingly supportive of innovative trial designs but require robust evidence to ensure patient safety and treatment efficacy.
The Road Ahead
The future of cancer immunotherapy is brimming with potential. Advances in genomics, artificial intelligence, and synthetic biology are poised to accelerate drug discovery and refine therapeutic strategies. Collaborative efforts among academia, biotech, pharma, and regulatory bodies will be key to translating scientific breakthroughs into clinical success.
As we move forward, cancer immunotherapy trials are not just aiming to extend life—they are striving to redefine what is possible in the treatment of cancer.
The new horizons in cancer immunotherapy trials reflect a bold and transformative era in oncology. By embracing personalized approaches, engineering next-generation therapies, and innovating trial designs, we stand on the brink of realizing the full promise of immunotherapy: turning cancer from a terminal diagnosis into a manageable, and potentially curable, disease.